-

ContiReflex®
Enhanced Artificial Urinary Sphincter -
Smart Reflex Balloon
Innovative “Smart Reflex Balloon” technology is revolutionizing the field of AUS. -

New Cuff Sizes
Variant cuff sizes for optimal adaptation to the patient’s urethral structure. -
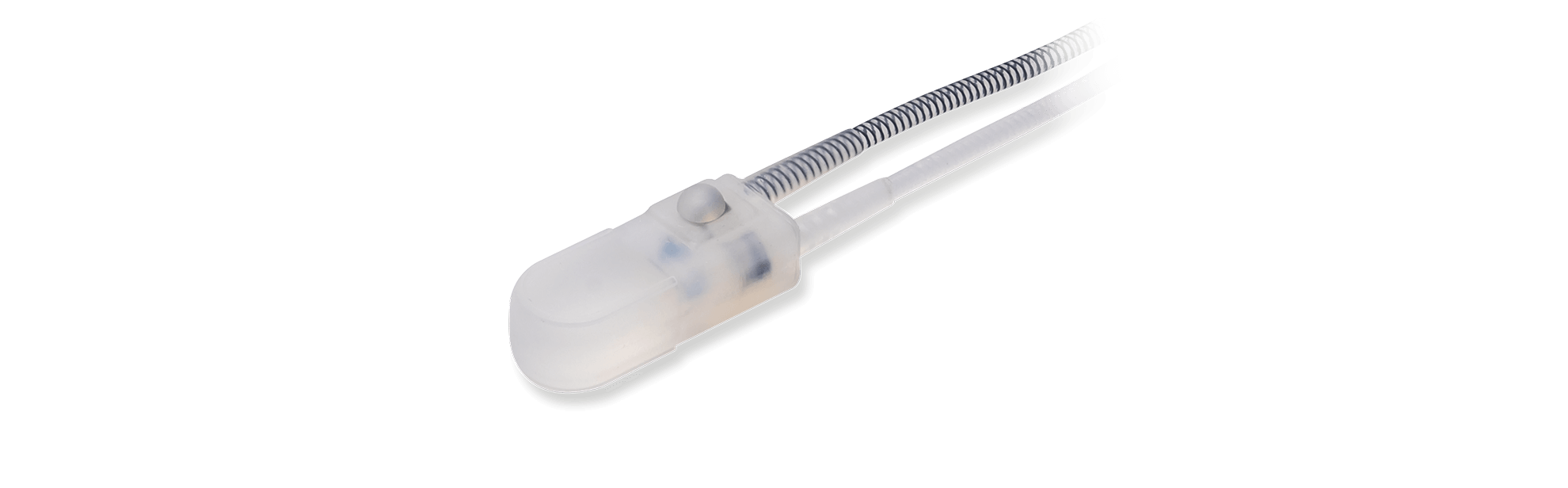
Control Pump
Effortless activation and deactivation mechanism.
-

ContiReflex®
Enhanced
Artificial Urinary Sphincter -

Smart Reflex Balloon
Innovative “Smart Reflex Balloon” technology is revolutionizing the field of AUS. -

New Cuff Sizes
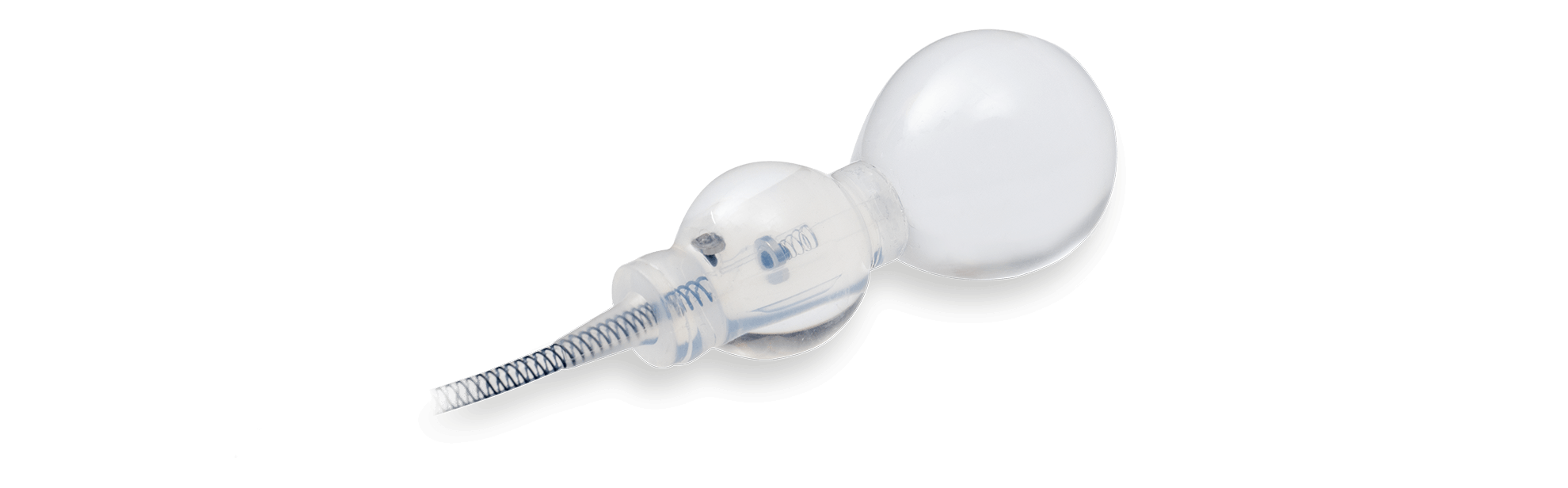
New and diverse occlusive cuff sizes for a surgeon-made fit to the patient’s urethral anatomy. -

Control Pump
Effortless activation and deactivation mechanism.
-
ContiReflex® Enhanced Artificial Urinary Sphincter is used to treat urinary incontinence due to intrinsic sphincter deficiency in cases such as incontinence following prostate surgery1
-
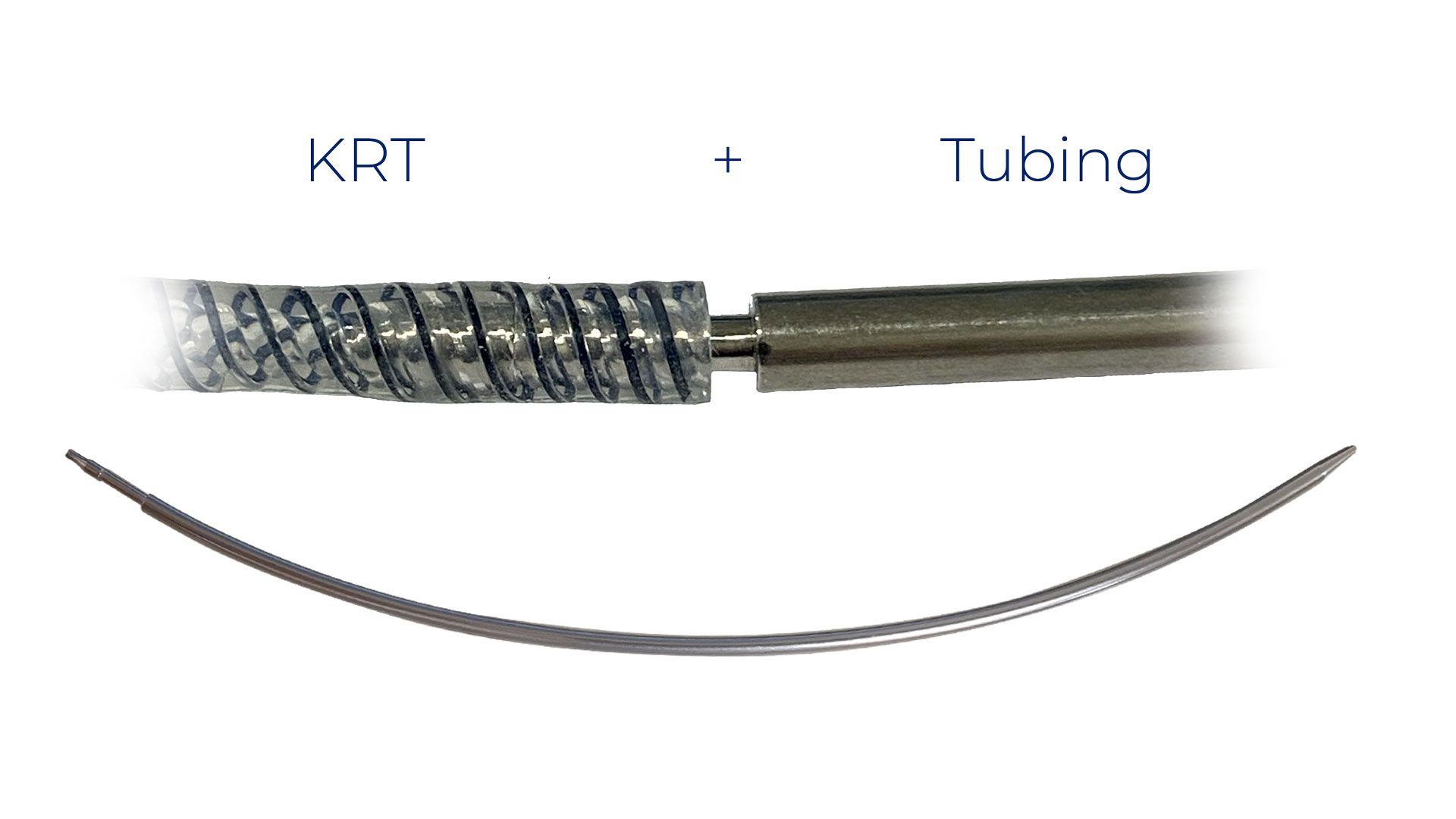
ContiReflex® Enhanced Artificial Urinary Sphincter‘s smart “Reflex Balloon” senses changes in intraabdominal pressure (IAP) and, in response, modifies the pressure on the urethra in response to this change in IAP.1
-
The Reflex Balloon has two bladders which allows the occlusive urethral pressure to be altered in response to the patient’s sudden Valsalva maneuver and, as a result, better protects the patient from stress incontinence. In effect, this means that cuff occlusion pressure is no longer limited by the pressure regulating balloon’s (PRB’s) labeled maximum pressure.
-
In addition, this two-bladder construction means the resting pressure of the balloon can be lower than competitive devices because protection from leakage is no longer reliant on the PRB’s labeled pressure. It is believed lower resting pressure of the PRB will prolong urethral viability decreasing the necessity for revision operations.
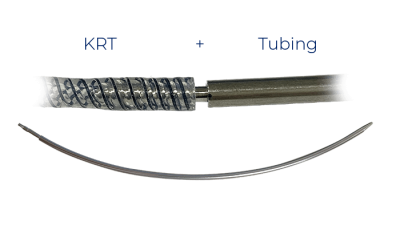
Smart Reflex Balloon
New Cuff Sizes
New and diverse occlusive cuff sizes for a surgeon-made fit to the patient’s urethral anatomy.
HydroShield™ Coating*
ContiReflex® features a hydrophilic coating on all external surfaces, including the pressure regulating balloon, allowing for compatibility with various antibiotics tailored to the patient’s needs. *:Ref
Control Pump
The ContiReflex® pump resembles competitive devices but differs because it is very easy to activate and deactivate.
FAQ
What is urinary incontinence?
Urinary incontinence (UI), sometimes referred to as “lack of bladder control,” is the involuntary loss of urine. Patients suffering from UI cannot control urine release from the bladder. Urinary incontinence is estimated to affect 1 out of 10 males, with increasing prevalence associated with aging.
What are the common causes of chronic stress urinary incontinence in men?
Eliminating overactive bladder muscles, weakened pelvic floor muscles, enlarged prostate, a disability or mobility, chronic illness, being overweight, and smoking.
This leaves only prostate cancer treatment and nerve damage.
What is Stress Urinary Incontinence (SUI)?
Stress urinary incontinence is the unexpected leakage of urine when an outside pressure occurs with activities such as heavy lifting, coughing, sneezing, laughing, or exercise.
This outside pressure causes the already weakened bladder to leak urine.
The bladder is held in place by the muscles and connective tissue in the pelvis. When these muscles are weak, the outside pressure can push the bladder downward, causing the urethra to open and the urine to leak out.
A weak or damaged sphincter may also cause stress urinary incontinence.
Is stress urinary incontinence a normal part of aging?
It is true that, stress urinary incontinence (SUI) is a normal part of aging for females, but it takes an event like trauma or surgery to give a man stress urinary incontinence.
How will my doctor diagnose urinary incontinence?
For diagnosis, your doctor will perform a physical examination and take your detailed medical history.
Depending on your medical history and physical examination findings, your doctor may require further testing.
Is stress urinary incontinence a side effect of surgical prostate treatment?
One of the most common side effects of radical prostatectomy is stress urinary incontinence.
It is expected for post-radical prostatectomy SUI to be resolved within one year following surgery. In some cases, patients may continue to experience SUI without any improvement over time. If you are having issues with bladder control and it is an issue six months after your procedure, you should see a specialized physician to seek medical advice and, if necessary, discuss your treatment options.
What are some of the treatment options for stress urinary incontinence (SUI)?
Remember that most stress urinary incontinence cases are treatable. Depending on the severity and the type of urinary incontinence, your doctor will decide on the best treatment option.
Commonly there are two treatment options:
1) Conservative treatment (e.g., medicines, special exercises)
2) Surgical treatment (e.g., Enhanced Artificial Urinary Sphincter)
What is an artificial urinary sphincter?
Enhanced Artificial Urinary Sphincter (AUS) is a medical device to treat stress urinary incontinence. Enhanced Artificial Urinary Sphincter is a surgical treatment option when non-surgical or behavioral treatment options fail.
Enhanced Artificial Urinary Sphincter placement is regarded as the “gold standard” in the surgical treatment of SUI.
A specialized physician (i.e., a urologist) will surgically place the artificial urinary sphincter in the body. Enhanced Artificial Urinary Sphincter will mimic the role of a healthy urinary sphincter (the two muscles controlling the exit of urine from the bladder through the urethra). The Artificial Urinary Sphincter will close the urethra preventing urine leakage. The patient will squeeze a pump in his scrotum to release the cuff over the urethra and void. The cuff will return to its closed state. The Enhanced ContiReflex® smart “Reflex Balloon” senses IAP; changes and modifies occlusive cuff pressure in real time. Cuff pressure is responsive to IAP changes and is no longer limited by the PRB’s labeled pressure capacity.
What are the benefits of ContiReflex® Enhanced Artificial Urinary Sphincter?
ContiReflex® Pump is easily manipulated, deactivated, and activated.
ContiReflex® Smart PRB adapts occlusive cuff pressure in a real-time manner.
ContiReflex® has a safe implantation via a single-incision penoscrotal approach.
ContiReflex® Enhanced Artificial Urinary Sphincter has more comprehensive occlusive cuff size options. This will enable your surgeon to choose the occlusive cuff that fits best with your urethral anatomy.
In some cases, double-cuff placement might be preferred. EasyClick™ Y-Connector will enable a double-cuff configuration of the device.
ContiReflex® Enhanced Artificial Urinary Sphincter incorporates a hydrophilic coating on all device surfaces. This hydrophilic coating will allow your surgeon to choose the aqueous solution she will dip into the device before implantation.
What should I expect for recovery after AUS implantation?
It is expected that a full recovery from artificial urinary sphincter implantation could take up to 6 weeks. Please keep in mind that every patient will have a different timeline for recovery. Your physician will manage your post-op care. You need to follow your physician’s suggestions for a speedy recovery. Your implanted Artificial Urinary Sphincter will be activated by your physician in your follow-up appointment, which is generally scheduled for four to six weeks after implantation.
Will others be able to notice that I have an Artificial Urinary Sphincter?
All components of the artificial urinary sphincter are concealed in your body and can not be noticed from the outside. Others will not know that you have an artificial urinary sphincter implanted unless you choose to disclose it.
Can Artificial Urinary Sphincter be used with Inflatable Penile Prosthesis simultaneously?
Aside from stress urinary incontinence, erectile dysfunction is another common side effect of radical prostatectomy surgery. If you are experiencing SUI and erectile dysfunction, consult a specialized physician. An artificial Urinary Sphincter can be used simultaneously with Inflatable Penile Prosthesis (e.g., Infla10 Three-Piece Inflatable Penile Prosthesis).
FAQ’s Disclaimer
Caution
References
1 Rigicon® ContiReflex® Enhanced Artificial Urinary Sphincter Instructions for Use.
2 Boysen, William, et al. “Combined Placement of Artificial Urinary Sphincter and Inflatable Penile Prosthesis Does Not Increase Risk of Perioperative Complications or Impact Long-term Device Survival.” Urology vol. 124 (2019): 264-270.