
Artificial Urinary Sphincter Solutions for Prostate Cancer Survivors

Understanding Urinary Incontinence After Prostate Cancer
Urinary incontinence, particularly stress urinary incontinence (SUI), is a prevalent and impactful consequence following treatments for prostate cancer. You're not alone, and today's technology has advanced significantly.
Prostate Cancer Treatment
Treatments like radical prostatectomy or radiation therapy can affect the urinary control mechanisms. Epidemiological data suggest that up to 60% of prostate cancer survivors may experience some degree of urinary leakage.
Impact on Quality of Life
Urinary incontinence can profoundly affect an individual's daily activities, social engagement, and overall emotional well-being. This condition significantly impacts quality of life and personal dignity.
Treatment Options
For persistent incontinence after prostate cancer treatment, artificial urinary sphincters are considered the gold standard solution when conservative options like pelvic floor exercises, pads, or medications are insufficient.
Why Artificial Urinary Sphincters Are the Gold Standard
For men experiencing persistent urinary incontinence after prostate cancer treatment, artificial urinary sphincters offer distinct advantages over other treatment options.
Key Benefits for Prostate Cancer Survivors:
- High Efficacy and Patient Satisfaction: Clinical studies consistently demonstrate high rates of continence and patient-reported satisfaction
- Significant Improvement in Quality of Life: Immediate and substantial enhancement in various domains of quality of life
- Restoration of Continence and Personal Dignity: Helping to restore a sense of normalcy, confidence, and personal dignity
"Patients undergoing AUS implantation typically experience significant improvements in their continence, leading to a drastic reduction in pad dependence."
"AUS implantation remains a highly effective treatment modality for SUI even in patients who have undergone prior pelvic radiation therapy for prostate cancer."
Rigicon's Advanced AUS Solutions for Prostate Cancer Survivors
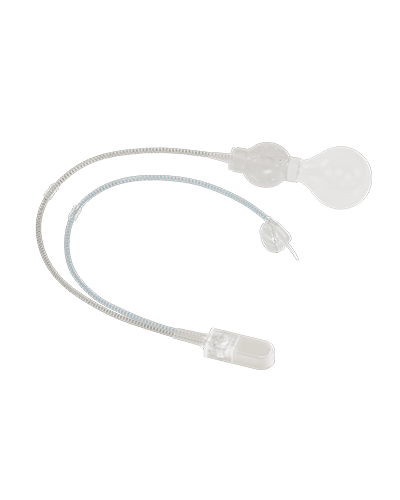
Introducing ContiReflex® Enhanced Artificial Urinary Sphincter
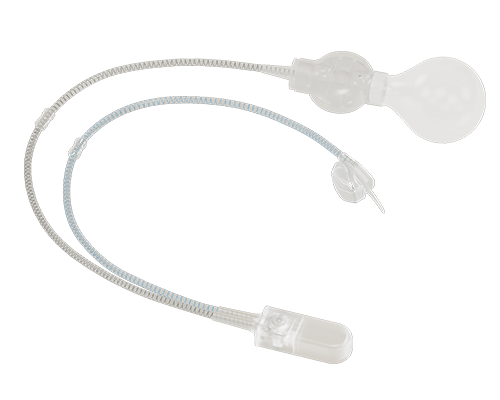
Smart Reflex Balloon
Senses changes in intraabdominal pressure (IAP) and dynamically modifies the pressure on the urethra, providing real-time protection against stress incontinence.
Dual Bladder Technology
Revolutionary two-bladder construction allows for lower resting pressure while maintaining superior protection, potentially prolonging urethral viability and reducing revisions.
Versatile Cuff Sizes
New and diverse occlusive cuff sizes for a surgeon-made fit to the patient's specific urethral anatomy, optimizing comfort and function.
HydroShield™ Coating
Hydrophilic coating on all external surfaces enables compatibility with various antibiotics tailored to each patient's specific needs.
Additional Advanced Features
EasyClick™ Connector
Tool-free connection system that simplifies the implantation procedure while maintaining a secure fit. For complex cases, the Y-Connector enables double-cuff configuration.
User-Friendly Control Pump
The ContiReflex® pump provides effortless activation and deactivation, with intuitive operation that makes daily use simple and reliable for patients of all dexterity levels.
Rigicon Duality
Compatible with Infla10® Inflatable Penile Prosthesis models, allowing simultaneous treatment of both erectile dysfunction and urinary incontinence - common side effects following prostate cancer treatment.
Frequently Asked Questions
Common questions from prostate cancer survivors considering artificial urinary sphincter options.
When is the appropriate time to consider an artificial urinary sphincter after prostate surgery?
Typically, AUS implantation is considered approximately 6 to 12 months following prostate surgery. This timeframe allows for the stabilization of continence status and ensures that conservative management options have been adequately trialed.
Are AUS devices effective after radiation therapy for prostate cancer?
Yes, AUS implantation remains a highly effective treatment modality for SUI even in patients who have undergone prior pelvic radiation therapy for prostate cancer. While radiation can present unique challenges, studies have demonstrated substantial improvements in continence and quality of life in this patient population.
What level of continence restoration can I expect from an AUS?
Patients undergoing AUS implantation typically experience significant improvements in their continence. Many individuals achieve social continence (requiring zero or one small security pad per day) or complete dryness, leading to a drastic reduction in pad dependence and a corresponding enhancement in their overall quality of life.
What is the recovery time after AUS implantation?
A full recovery from artificial urinary sphincter implantation typically takes up to 6 weeks, though individual timelines may vary. Your physician will manage your post-operative care and activate your implanted AUS during a follow-up appointment, usually scheduled 4-6 weeks after the procedure.
Will others be able to notice that I have an Artificial Urinary Sphincter?
All components of the artificial urinary sphincter are concealed within your body and cannot be noticed from the outside. Others will not know that you have an artificial urinary sphincter implanted unless you choose to disclose it.
Can an AUS be used with a Penile Prosthesis simultaneously?
Yes. Both stress urinary incontinence and erectile dysfunction are common side effects of radical prostatectomy. If you're experiencing both conditions, the ContiReflex® Artificial Urinary Sphincter can be used simultaneously with an Inflatable Penile Prosthesis such as Rigicon's Infla10® Three-Piece system.
Ask Your Surgeon About Rigicon
Schedule a consultation to discuss whether Rigicon's innovative artificial urinary sphincter options are right for you after prostate cancer treatment.
Find ResourcesDiscover More

Clinical Evidence
Peer-reviewed publications and clinical evidence from the frontiers of prosthetic urology
Prosthetic Urology FAQs
Evidence-based FAQs on artificial urinary sphincters, penile and testicular prostheses—grounded in peer-reviewed research and the latest international guidelines.

Rigicon Blog
Explore expert insights on artificial urinary sphincters, erectile dysfunction, penile implants, and men's urological health.